Abstract
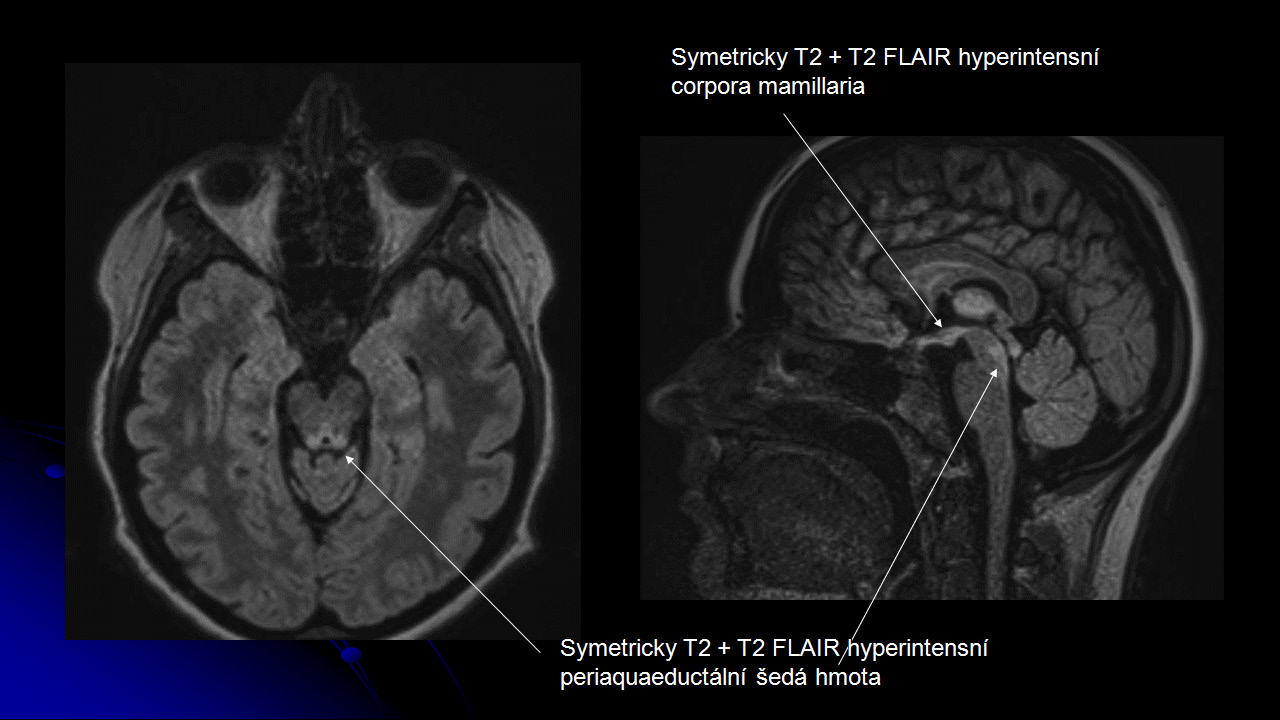
The authors report a case study of a 24-year-old female patient after sleeve gastrectomy with subsequent manifestation of Wernicke’s encephalopathy. After 5 weeks following the surgery, which were uneventful, the patient was repeatedly hospitalized in the surgical department for extreme vomiting; however, her health status rapidly improved with infusion therapy followed by careful re-alimentation. At the same time, her GIT was closely examined without any clear finding. Problems progressively deteriorated into neurological manifestations. The final diagnosis was established by MR imaging of the brain. In addition, the patient’s condition was complicated by sudden febrile status with elevated CRP values; therefore, with regard to the unclear CT finding in the abdominal cavity, a laparoscopic revision was made 8 weeks after the primary surgery. The patient survived thanks to the final correct diagnosis and administration of adequate therapy in the form of thiamine substitution. After 30 days following the last admission, the patient was discharged for home treatment in a satisfactory health condition. The aim of the case study is to describe the onset of atypical symptoms in a patient following bariatric surgery – particularly from the point of view of a surgeon – and difficult and prolonged diagnosis of this syndrome due to its relative rarity, also from the point of view of other colleagues with various specializations who participated in the establishment of the diagnostics.