Abstract
Introduction: Pulmonary embolism is a life-threatening condition that causes obstruction of the pulmonary arteries by an embolus, most often originating from the venous system of the lower limbs or pelvic veins. Depending on the extent of the embolism, an acute right-sided heart failure may result, with subsequent death. Paradoxical embolism is a condition in which a venous thrombus is embolized into the systemic circulation arteries by a right-to-left heart shunt. This condition most commonly occurs in the interatrial septum. The aim of treatment for pulmonary embolism is to remove the obstruction of the lung. Depending on the extent of the embolism and the patient’s hemodynamic status, thrombolytic or surgical treatment can be chosen. Thrombolytic therapy has become the basis of treatment for all types of acute pulmonary embolism. Currently, open surgery is indicated in hemodynamically unstable patients with massive pulmonary embolism, and increasingly frequently in submassive embolism where thrombolytic therapy is not effective or contraindicated.
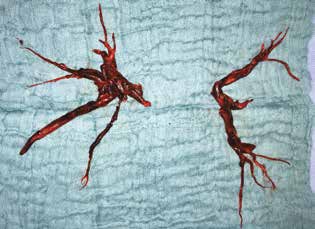
Case report: The case report describes a less common condition of pulmonary and concurrently systemic embolization in the subclavian artery. Thrombolytic therapy was contraindicated in this case due to the high risk of secondary embolism to the brain. Surgical embolectomy was performed from the pulmonary arteries simultaneously with direct embolectomy from the subclavian and brachiocephalic artery. The surgical management of acute pulmonary embolism is a suitable method of treatment for both massive pulmonary embolism where the procedure is performed as a life-saving indication, and submassive embolism where less invasive treatment would not be effective.
Conclusion: Direct embolectomy of subclavian and brachiocephalic artery is associated with minimal risk of iatrogenic embolism into the arteries supplying the brain compared to indirect embolectomy performed from the cubital or brachial artery.