Abstract
Introduction: Overweight and obesity are recognized as risk factors for many health-related disorders like diabetes, cardiovascular disease and malignancy. On the other hand, according to recent studies, they may be a favorable prognostic factor in patients treated for various chronic diseases. Patients with increased body mass index (BMI) have a lower mortality rate, which is known as the “obesity paradox”. Overweight and obese patients, as reported by several papers, also have better outcomes after surgery. The aim of our study was to evaluate this somewhat surprising phenomenon on our group of patients.
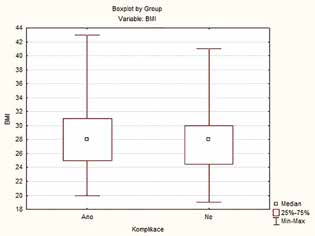
Methods: The medical records of patients diagnosed with colorectal cancer who were treated with resection and primary anastomosis from 1 January 2010 to 31 December 2017 were retrospectively analyzed. Patients after multivisceral resections or with lacking data were excluded. We did not evaluate two underweight patients. The BMI classification of the World Health Organization was used. Postoperative complications, anastomotic leak, mortality and length of stay in hospital were investigated.
Results: 225 patients were included. 56 (24.9%) patients had normal weight – group A, 98 (43.6%) patients were overweight – group B, 58 (25.7%) patients had class I obesity – group C, 9 (4%) patients had class II obesity and 4 (1.8%) patients class III obesity – together they form group D. The groups did not significantly differ in age, sex, comorbidities, cancer stage and locality. Complications occurred as follows: A–29%; B–25%; C–36%; D–55%. Anastomotic leak: A–9%; B–4%; C–9%; D–15%. Mortality: A–5%; B–2%; C–2%, D–0%. Average length of stay: A–11.7 days; B –11.3 days; C–12.6 days; D–47 days. We did not observe any statistically significant difference.
Conclusions: Overweight surgical colorectal cancer patients had the lowest incidence of complications, anastomotic leak and the shortest length of stay. Obesity was associated with more complications but reduced inhospital mortality. Probably due to the relatively small number of patients, we did not prove any statistically significant difference.