Abstrakt
Úvod: Aorto-ilická ateroskleróza je nejlépe léčena endovaskulárně angioplastikou/stentem nebo chirurgicky bypassem, podle závažnosti postižení. Aorto-ilická endarterektomie byla často prováděna až do 80. let, nicméně může být stále použita v případě selhání či kontraindikace standardních metod. Cílem práce je retrospektivní zhodnocení zkušeností jednoho cenra s pánevní endarterektomií.
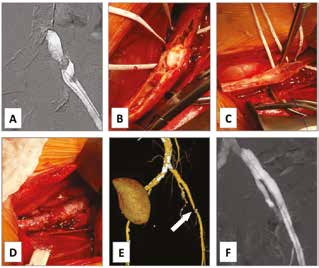
Metodika: Sedm pacientů o průměrném věku 60±8 let (57−68 let) podstoupilo pánevní endarterektomii v letech 2013−2018. Kategorie končetinové ischemie podle Rutherforda byly 2 (střední klaudikace) 3x, 3 (těžké klaudikace) 2x, 4 (klidová bolest) a 5 (gangréna prstů). Důvodem k endarterektomii bylo: pozdní in-stent pánevní okluze u onkologického pacienta, neúspěch nebo komplikace předchozí endovaskulární léčby krátké pánevní stenózy 2x, vysoké riziko infekce protézy u dlouhé pánevní okluze a krátký pánevní uzávěr 3x. Dva pacienti byli po předchozí orgánové transplantaci na imunosupresi.
Výsledky: Technický uspěch byl 100 %. Nedošlo k perioperační (≤30 days) mortalitě nebo amputaci. Průměrné sledování je 17 měsíců (1,1 měsíce− 3,3 roky). Jeden pacient potřeboval tibiální bypass 1 měsíc po endarterektomii pro zhojení gangrény. Jedna pacientka podstoupila pánevní stenting pro symptomatickou restenózu po 8 měsících. U všech došlo ke klinickému zlepšení a zotavení z končetinové ischémie. Dva pacienti zemřeli na nádorové onemocnění se zachovanou končetinou 1,1 měsíce a 3,1 roku po operaci. Pět ostatních dosud žije bez obtíží s průchodnou rekonstrukcí.
Závěr: Aorto-ilická endarterektomie je vitální revaskularizační technika u vybraných pacientů v případě nevhodnosti ostatních metod.