Abstract
Introduction: Minimally invasive methods for esophagectomy have been introduced to reduce postoperative complications. This paper compares open transhiatal esophagectomy and minimally invasive hybrid esophagectomy. Both methods have different extents of lymphadenectomy, transhiatal esophagectomy being considered less radical.
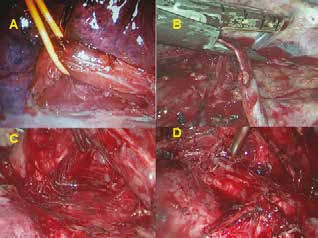
Method: A single-centre retrospective study comprised 39 patients subjected to transhiatal esophagectomy and 25 patients subjected to hybrid esophagectomy combining thoracoscopy with laparotomy and cervical anastomosis. All patients were operated for middle and distal third carcinoma of the esophagus, including cardia (Siewert II), in the period of 2006−2016 at the Surgery department of Nový Jičín hospital. The data of both groups, in particular the incidence of early postoperative complications and the number of dissected lymph nodes, were statistically compared. Complications are reported according to the International Consensus on Standardization of Data Collection for Complications Associated with Esophagectomy.
Results: The duration of operation was significantly longer in the group that underwent hybrid resections (345 vs. 240 min, p<0.001). The number of dissected lymph nodes was comparable in both groups (15 vs. 16, p=0.072). Postoperative pulmonary complications were lower for hybrid operations (16% vs. 30.8%, p=0.243). The most common complication of transhiatal esophagectomy was pleural effusion requiring drainage, which occurred in 7 patients. The most common pulmonary complication of hybrid procedures was respiratory failure, which occurred in 3 patients. Anastomotic leak occurred in 5 patients after transhiatal esophagectomy and in one after thoracoscopic resection (12.8% vs. 4%, p=0.391). 30-day and 90-day mortality was nonsignificantly lower for hybrid resections (0% vs. 5.1%, p=0.516 and 4% vs. 10.3%, p=0.64). Following transhiatal esophagectomy, two patients died as a result of respiratory complications, one died from necrosis of the gastric tube and one from acute myocardial infarction. In the hybrid group, one patient died from respiratory failure. Hybrid resection exhibited lower morbidity (36% vs. 59%, p=0.123). The number of overall complications, irrespective of their severity according to the Clavien-Dindo classification, was statistically in favor of hybrid resection (11 vs. 30, p=0.015).
Conclusion: In our study, we found that thoracoscopic hybrid resection was a feasible and well-executable method, with a statistically lower incidence of postoperative complications. Thoracoscopy allows lymphadenectomy to be performed to sufficient extent. The large number and various combinations of esophagectomy techniques make it difficult to evaluate and compare the outcomes of individual methods. Preference for a specific resection technique within a given surgical department remains an important factor as clear recommendations for esophageal resections do not yet exist. However, the use of minimally invasive techniques in esophageal resections is gradually becoming a standard.