Abstract
Introduction: No consensus exists as yet regarding the optimal extent of surgery on the lymph nodes in breast cancer patients after neoadjuvant treatment. In addition to axillary dissection and sentinel lymph node biopsy (SLNB), a new approach called Targeted Axillary Dissection (TAD) was introduced. It requires the marking of metastatic nodes before the neoadjuvant treatment.
Method: A retrospective observational study on patients with breast cancer and neoadjuvant chemotherapy treated surgically at a single institution in 2017.
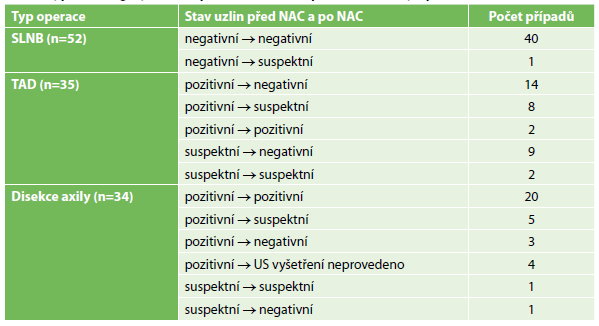
Results: The analysis included 121 cancers in 120 patients. Clinical regression of lymphadenopathy occurred in 29 out of 74 cases. Axillary dissection was performed 34x, SLNB 52x and TAD 35x. In TAD procedures, the marked lymph node was found 30x and was among the sentinel nodes in 19 cases. No case occurred in which the marked node was assessed as negative with a metastasis found in the other nodes. On the contrary, there were 3 cases with negative sentinel nodes whereas the marked node was positive. Out of 74 cases with initially pathologic nodes, 23 patients were spared axillary dissection.
Conclusion: Clinical assessment of the lymph node status is rather inaccurate. In cases with initially pathologic nodes we recommend marking of the most explicit metastatic node to enable TAD. The marked node is likely to reflect the status of the lymph nodes after neoadjuvant treatment more accurately than common sentinel nodes. A considerable proportion of patients can be spared axillary dissection in this way. However, the long-term oncologic safety of TAD still needs to be verified.