Abstract
Introduction: Chronic back pain (CBP) is a very common symptom. Multiple modalities are used in its evaluation. However, according to current evidence, none of them can be used with certainty to predict the success of fusion surgery. Given the growing experience with bone tissue examination using the methods of nuclear medicine, we have used this possibility in patients with CBP without disc herniation, degenerative spinal stenosis or instability.
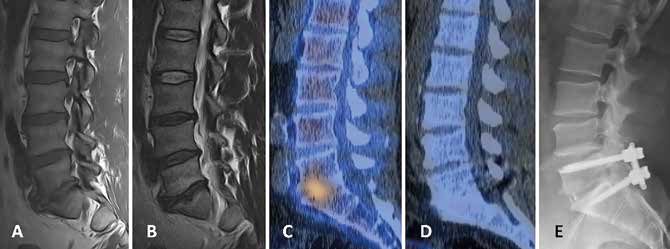
Case reports: We present case reports of 11 patients who underwent lumbar fusion (during two years period) for degenerative disc disease or facet arthropathy with adequate activity on PET or SPECT/CT examination. Rolland-Morris Questionnaire (RMQ), Oswestry Disability Index (ODI), and Visual Analogue Scale (VAS) were filled out pre-operatively and 24 months after surgery.
Results: Six patients after one-level stabilization for active osteochondrosis and one for active facet arthropathy improved on average by 82% (64–92%) in RMQ, by 72% (48–100%) in ODI and 75% (55–100%) in VAS. Results in cases after multilevel stabilizations were slightly worse, but still very significant in most parameters. Only one patient with the most severe morphological and clinical findings did not benefit from surgery.
Conclusion: In 10 out of 11 patients, the lower back pain and quality of life improved significantly after lumbar fusion performed in levels diagnosed by PET or SPECT/CT. These methods certainly have their place in the evaluation of CBP, especially in the case of unclear findings or multiple degenerative changes.