Abstract
Introduction: The main cause of postoperative pain after abdominal surgery is the wound where laparotomy is made. Recently, laparoscopic procedures
have become common in colorectal surgery. Although improving the tolerance of the surgery, postoperative pain management still remains
a discussed problem. The use of an epidural catheter used to be generally recommended in the open surgery era; however, an ideal strategy for
postoperative analgesic therapy after laparoscopy remains unclear. Reduced administration of opioid analgesic drugs after colorectal resection is
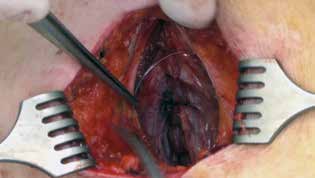
a generally accepted goal. Preperitoneal catheter insertion for continuous local anaesthetic (LA) infusion in the wound after surgery is a simple
alternative to other pain management methods.
Methods: Retrospective analysis of analgotherapy outcomes in patients undergoing laparoscopic colorectal resection procedures, divided in three
patient groups according to the type of analgesia: Group 1: use of a catheter for local wound infusion (KAT) n=73; group 2: epidural analgesia (EPI)
n=23; and control group 3 with combined parenteral and subcutaneous analgesia (CON) n=66. The main objective of this study was to analyse
postoperative pain and the consumption of opioid analgesics in the first three days from the surgery and the incidence of any complications related
to the analgesic therapy.
Results: Opioid consumption in KAT and EPI groups was significantly lower compared to CON in the first 72 hours from the surgery. The lowest
postoperative pain was measured in the EPI group. Subjective perception of pain, measured using VAS, was not significantly different between the
KAT and CON groups. In KAT patients, vomiting was statistically less frequent than in CON patients. There was no significantly different incidence
of paralytic ileus in the KAT and CON groups and no paralytic ileus was observed in the EPI group. There was no increased incidence of SSI (surgical
site infections) in the KAT group compared to the other groups.
Conclusion: The use of the catheter was assessed as safe. Insertion and management of the catheter is unsophisticated, and we did not observe any
complications in terms of application of the catheter or toxic side effects of the LA. The use of the catheter clearly reduced opioid administration
in the postoperative period compared to the control group (CON) with combined parenteral and subcutaneous analgesics. The best pain control
measured using the visual analog scale (VAS) was observed in the EPI group.