Abstract
Introduction: Over the last decades outcomes for rectal cancer surgery have improved with increasing survival and lower recurrence rates. Nevertheless, functional disorders are still frequent. Low anterior resection with total mesorectal excision (TME) in patients with rectal cancer has improved oncological outcomes. However, most of them will have significant changes in quality of life, including varying degree of bowel dysfunction. Aim of this study was to analyse prevalence of LARS (low anterior resection syndrome) in patients with rectal cancer after miniinvasive restorative resection and to define its risk factors.
Methods: Between March 2016 and June 2018, patients who underwent elective miniinvasive (laparoscopic or robotic) rectal resection were enrolled. Bowel dysfunction was evaluated by LARS questionnaire and filled out 6, 12, and 24 months after primary operation or after ileostomy closure. 98 patients completed the questionnaires – 58 laparoscopic operations, 34 robotic and 6 open procedures. 69 patients underwent TME, tumor-specific mesorectal excision 21 patients. 8 patients underwent transanal TME. The clinical characteristics, surgical perioperative and postoperative outcomes did not differ between these groups. Only, significantly more patients underwent neoadjuvant radiotherapy in the robotic group (p=0.004).
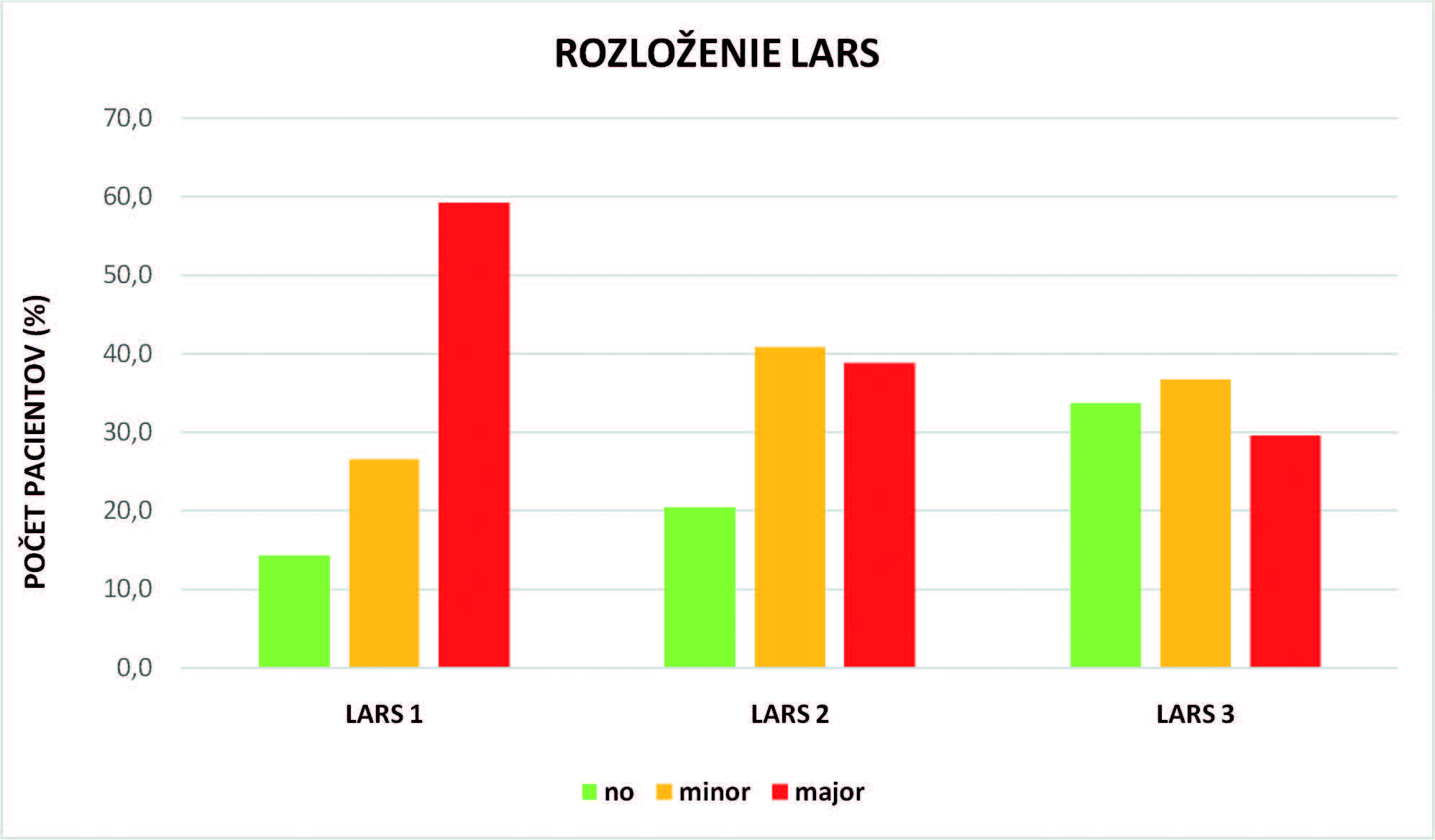
Results: 59.8% patients reported major LARS 6 months after surgery and 29.7% after 24 months. Protentional risk factors are age (p<0.05), tumor height (p<0.001), time from stoma resection (p<0.05), neoadjuvant (p<0.001) and adjuvant therapy (p<0.05).
Conclusion: Prevalence of LARS is high. It is underestimated, although an important factor. Radiotherapy and TME are significant risk factors of major LARS.