Abstract
Introduction: Radiofrequency ablation is an effective management modality for irresectable primary and secondary liver tumors. Some serious complications have been reported including diaphragmatic hernia. Diaphragmatic hernia is the protrusion of abdominal viscera into the thoracic cavity through a diaphragmatic defect and usually classified into congenital and acquired. After RFA, diaphragmatic hernia is a rarely-reported complication.
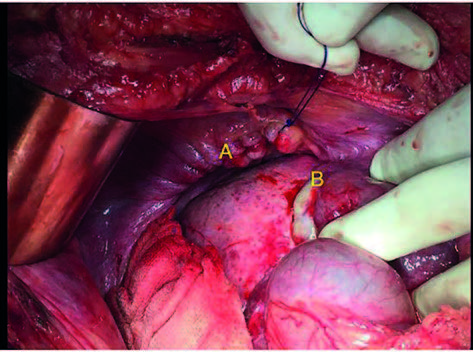
Case report: A 62-year-old male patient, known to have liver cirrhosis on top of hepatitis C virus, presented to the emergency department with generalized abdominal pain and vomiting four months after having a RFA procedure for a liver tumor in segment VIII. Computed tomography showed diaphragmatic hernia with strangulated terminal ileum in the chest. Emergency laparotomy was performed with resection of an ileal segment and creation of double barrel ileostomy. The patient was discharged in a good condition after tolerating oral intake.
Conclusion: Radiofrequency ablation is an effective modality for management of the primary and secondary liver tumors. Despite its safety, some complication may happen owing to its thermal effect and the associated patient’s general condition. Many techniques have been described to decrease its thermal injury. Diaphragmatic hernia is a rare complication after RFA. Its clinical presentation may be confusing and it may occur as early as one month after RFA. Its diagnosis depends mainly on computed tomography. Emergency surgical management is the standard approach