Abstract
Introduction: A bulky retrosternal goiter means for the surgeon to consider an extracervical approach, usually from a partial sternotomy.
Methods: Retrospective evaluation of a group of thyroid operations requiring sternotomy in a ten-year period (year 2012–2021), in an attempt to predict the need for sternotomy.
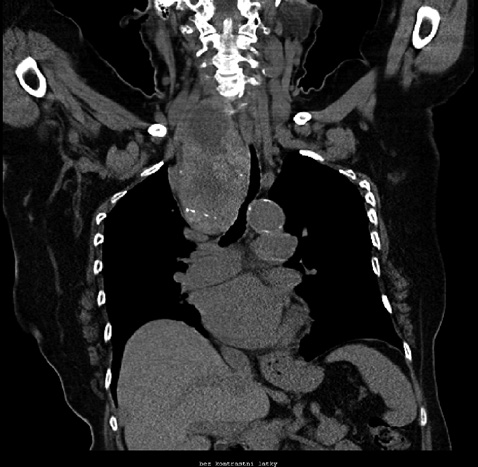
Results: We performed a total of 1254 thyroid operations, with partial sternotomy required in 11 cases (0.88%): in 6 women and 5 men aged 43–84 years (mean 73.1 years). For these, 3 total thyroidectomies and 6 hemithyroidectomies (lobectomies) were performed. In 2 cases, we operated on the mediastinal residue, or regenerate, after a previous thyroidectomy from the cervical approach. The duration of hospitalization was 5–14 days, once there was bleeding with the need for operative revision, otherwise the procedures were without complications, including phonation. The border of the lower part of the thyroid gland in relation to the upper border of the aortic arch was in the range of +20 to -22 mm. The mean was -8.5 mm.
Conclusion: All sternotomy thyroidectomies performed by us had a close relationship to, or overlapped with the upper line of the aortic arch. Significantly retrosternal propagating goiters are mostly eufunctional (81.9 % in our group) and develop in patients in the seventh or eighth decade of life. Therefore, if only one lobe propagates intrathoracically, a hemithyroidectomy is sufficient. A carcinoma is rarely present; in one case in our group. We believe that the necessity of sternotomy cannot be accurately predicted, but it is necessary to be prepared for it, especially in the case of a goiter exceeding the level of the aortic arch. In case of greater retrosternal propagation, it is certainly appropriate to perform a CT, for surgical reasons (possibility of sternotomy, risk of leaving part of the gland) and anesthetic reasons (compression and deviation of the trachea)